Hospitals face increased need amid pandemic to improve patient throughput
An acute care hospital cannot begin to be able to deliver cost-effective care if it lacks a fully coordinated approach for moving patients from admission to discharge.
Lower admissions. Higher patient days. Longer-than-average length of stay (LOS) in acute care. These are among the significant challenges U.S. acute care hospitals face as a result of the COVID-19 pandemic.
This problem is in part a consequence of the processes and protocols hospitals put in place to keep patients and staff safe throughout the pandemic. But it was exacerbated by the unanticipated challenges of personal protective equipment (PPE) shortages and significant increases in agency staffing and associated costs. Amid these challenges, it has become critical for hospitals to find ways to reduce LOS and enhance patient throughput. Only through such effort can they ensure their future financial and operational success and fully realize their mission of caring for the patients in their communities.
The struggle to deliver timely care
Since the start of the pandemic, hospitals have struggled to deliver care to patients in a timely manner. Dealing with longer stays in the hospital has cut into their inability to accept transfers. Meanwhile, patients face long waits in the emergency department (ED), as operational constraints have made it extremely difficult for hospitals to achieve the four-hour turnaround time for patients in the ED recommended under Medicare guidelines.
Moreover, patients who await discharge to a post-acute care setting can expect to spend significantly longer in the hospital than those awaiting discharge to the home-care setting. There are three fundamental reasons for this difference:
- An increased number of payers require prior authorization for discharge to post-acute care.
- Staffing shortages in care management departments make it more difficult for hospitals to prepare patients for discharge to the post-acute care environment.
- Most communities have limited resources to meet the increased demand for post-acute care facilities, given that both hospitals and post-acute care facilities are contending with the same staffing challenges.
These barriers, combined with supply shortages and rising input costs on labor, make maintaining effective patient throughput in short-term acute care facilities an operational puzzle for administrators of these facilities.
Hospital finance leaders have a meaningful role to play in solving this puzzle. But to fulfill that role, they must clearly understand what is involved in patient throughput, including the people and processes that are needed to ensure patients do not encounter bottlenecks on their journey from hospital admission to discharge. These considerations are addressed in the sidebar — {design: state location of sidebar}. With this understanding, finance leaders can begin to advocate best practices that can enable a hospital to optimize patient throughput, thereby ensuring patients have a positive experience with their hospital care.
Best practices in optimizing patient time in the hospital
There are many solutions for addressing the barriers that arise throughout a patient’s hospital journey. Reducing LOS and improving patient throughput requires attention not only to the basic process steps involved with moving patients through the hospital but also to considerations around clinical variation and care management. These interlocking factors are depicted in the exhibit below.
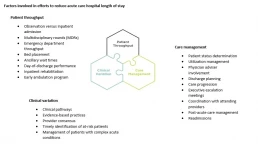
The foremost concern is ensuring the patient receives the right care. Patients who have been assigned the wrong status may experience delays in treatment because of requirements imposed by their payers or because the diagnosis on which the patient’s status is based is of lower priority than the diagnosis that more appropriately describes the patient’s condition. Confirming that the patient is in the right status at the right time allows for the appropriate treatment to begin at the right moment. Moreover, ensuring the patient is in the right status from the point of entry helps to prevent confusion over copays, deductibles and out-of-pocket expenses once the patient leaves the hospital, regardless of the setting.
It is important to see throughput as a journey, not a destination. Although clinicians must take the lead, the ability to effectively address throughput challenges requires a team-based approach involving participation by the care team, operations, finance and transport.
Finance leaders can play an important role by advocating for adoption of five leading practices that efficient hospitals use daily to promote effective throughput, described below and depicted in the exhibit below.
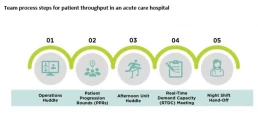
1 Operations huddle. The house operations huddle should be held in the morning, after shift change. Executives should attend this huddle for escalation purposes, while directors from all departments report out constraints they expect for the day, assess house-wide bed availability and address staffing shortages and safety and quality issues.
2 Patient progression rounds. The next step in the throughput cycle is for care team members to participate in unit-based patient progression rounds, with the goal of reviewing each patient’s treatment plan, discharge objectives and barriers to discharge. The entire care team must participate in this process to ensure patients will appropriately progress through their care while also being prepared for discharge. Once the day’s rounds are completed, the care team will be able to identify how many patients will be discharged that day and mitigate any barriers to those discharges.
3 Afternoon unit huddle. In the afternoon, care teams should gather for unit-based afternoon check-ins. This huddle gives each team an opportunity to quickly follow up on the action items from rounds, touch base on discharges expected later in the day and inform unit leaders of specific discharge barriers requiring their intervention.
4 RTDC meeting. Once the unit leaders have resolved the barriers to the extent possible, the larger team gathers for a second house-wide huddle, called the real-time demand capacity planning meeting (RTDC). The goal of the RTDC is to communicate where the remaining bottlenecks to patient throughput are and immediately address them with the appropriate leaders. Unit-based leaders should report out remaining discharges for the day, to enable transport managers to appropriately schedule the discharges and ensure requisite staff will be available. Outstanding constraints from the morning bed-huddle should be followed up during this meeting. Staffing should be addressed, test results expedited and preparations for morning discharges begun as well.
5 Night shift handoff. At end of the day, during shift change, discharge directives must be incorporated into handoff. Identifying a discharge readiness assessment and/or process into shift change continues the throughput cycle from day into night. The better the night shift understands throughput and feels the urgency to plan for discharge, the more efficient the hospital will be in continuity of its throughput. Although it may seem that a great deal of time is being spent on managing the movement of patients, it is time well spent, because next to patient safety, it is the care team’s most important responsibility.
Other steps for promoting cost effectiveness
In addition to these proposed solutions, hospital finance leaders should devote attention to other ways that hospitals can reduce LOS and streamline throughput, including:
- Focusing on improving care of patients with complex conditions who typically have long LOS
- Advocating for reducing clinical variation through development of pathways and protocols for standardized disease states
- Collecting data to track and trend discharge barriers, to continuously work toward the removal of common barriers to discharge
These solutions and leading practices are just a few pieces to the larger puzzle that hospitals must solve to improve operations and efficiencies. Success in managing throughput will remain elusive, however, without the understanding and support of the entire organization, where everyone is working toward a common goal. The pandemic may have made this truth more evident, but it remains fundamental to the success of our healthcare system under all circumstances.
Patient throughput: What it means and who is responsible for it
Patient throughput in the hospital is more than just admission to discharge for each patient. It also is everyone’s responsibility in the hospital setting. And it poses a particular challenge when one considers that patients can arrive at any of multiple portals of entry, each with their own admission protocols.
Consider the following scenario of a medical inpatient.
This patient arrives in the emergency department (ED). The emergency medicine providers determine the patient will be admitted as an inpatient to a med/surg floor – technically, this patient’s inpatient throughput timer begins when the provider writes the admission order.
Once the patient is transferred to the inpatient unit, hospitalists and specialists begin working to determine a diagnosis and projected prognosis for the patient. At the same time, the case management/discharge planner is learning about patient’s circumstances and the extent to which family support is available, while the therapy team is assessing the patient for additional discharge needs.
Once a preliminary diagnosis is assigned to a patient chart, the diagnosis corresponds to an expected geometric mean length of stay (GMLOS) per CMS. The care team continues to work together toward an expected discharge date, which should align with the expected LOS. It is important to note that a diagnosis may not be assigned to the patient until they are nearly two days into their stay. It therefore is crucial for the care team to know how long a typical patient stay would be based on the projected diagnosis, to proactively plan for discharge when no GMLOS is available.
A critical process
Throughput is the backbone for hospital LOS. It is critical to have systemwide, multidisciplinary buy-in to throughput, with all care team members being focused on treating the patient and transitioning them to the next level of care. A hospital’s ability to get patients in and out of the hospital is critical to hospital operations. In today’s environment, hospitals are experiencing a high demand in the ED as well as for elective procedures that were postponed during the pandemic and transfers requiring a higher level of care. Without efficient processes and operational support to help drive throughput, hospitals will experience significant constraints.
Implications of reduced LOS
Efforts to reduce LOS have both financial and quality implications. For payers that pay per a diagnostic-related group schedule, that payment amount reflects the patient’s expected level of care based on their diagnosis. Meeting the expected LOS ensures the payment will cover the cost of caring for the patient, and it will create capacity that ultimately allows the hospital to continue delivering care to other patients in the community.
Reduced LOS also is beneficial to the patient receiving care. Research shows that the longer patients stay in the hospital, the more susceptible they are to unsafe conditions, putting them at risk for hospital-acquired conditions and other complications. These are negative quality indicators for the hospital, as well. Efficient patient care, coupled with clear communication, are paramount not only to moving patients efficiently from admission to discharge, but also enhancing the overall patient experience. As the exhibit below shows, short-term acute care hospitals in the 20th percentile in terms of quality are able to discharge a high percentage of patients to home or self-care.
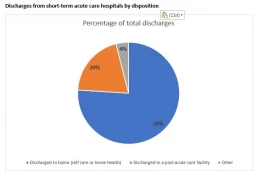
Based on top 20th percentile from Medicare Provider Analysis and Review data, 2020
